Understanding Osteoporosis & Preventing Fractures in Seniors

Osteoporosis, a condition marked by weakened bones, significantly elevates fracture risk in older adults, necessitating comprehensive strategies focused on dietary, lifestyle, and medical interventions to boost bone density and prevent debilitating breaks.
Navigating the complexities of aging brings forth a myriad of health considerations, with bone health frequently overlooked until a debilitating event occurs. In this context, staying informed about Updated Information: Understanding Osteoporosis and Preventing Fractures in Seniors becomes paramount.
The Silent Threat: Unraveling Osteoporosis in Older Adults
Osteoporosis, often dubbed the “silent thief,” is a progressive disease characterized by a reduction in bone mass and deterioration of bone tissue, leading to increased bone fragility and a higher risk of fractures. This condition disproportionately affects seniors, transforming everyday activities into potential hazards. Understanding its insidious nature is the first step toward effective prevention and management.
The skeletal system, far from being static, is a dynamic structure constantly undergoing a process of remodeling, where old bone tissue is removed (resorption) and new bone tissue is formed (formation). In younger years, bone formation outpaces resorption, leading to increased bone density. However, as individuals age, particularly post-menopause in women and gradually in men, this balance shifts. Resorption begins to outpace formation, leading to a net loss of bone mass.
Key Factors Contributing to Osteoporosis
Several factors contribute to the development of osteoporosis in seniors, extending beyond the natural aging process. Identifying these risk factors is crucial for early intervention and personalized prevention strategies.
- Age: Bone density naturally decreases with age, making older adults inherently more susceptible.
- Gender: Women, especially after menopause, are at a higher risk due to the sharp decline in estrogen, a hormone vital for bone maintenance.
- Genetics: A family history of osteoporosis or fractures can significantly increase an individual’s risk.
- Nutritional Deficiencies: Inadequate intake of calcium and vitamin D, both essential for bone health, weakens the skeletal structure over time.
Beyond these primary factors, lifestyle choices, certain medical conditions, and medications can also accelerate bone loss. For instance, prolonged immobility, smoking, excessive alcohol consumption, and chronic inflammatory diseases like rheumatoid arthritis can compromise bone integrity. Moreover, certain drugs, such as corticosteroids, taken long-term, are known to contribute to bone demineralization.
The insidious nature of osteoporosis means it often goes undiagnosed until a fracture occurs. These fractures, particularly of the hip, spine, and wrist, can lead to severe pain, disability, and a significant decline in quality of life. For seniors, a hip fracture can be particularly devastating, often leading to a loss of independence and, in some cases, increased mortality. Therefore, awareness and proactive measures are not just beneficial but imperative for maintaining health and functional independence in later life.
Diagnostic Advances: Pinpointing Bone Weakness Early
Early diagnosis of osteoporosis is pivotal in preventing fractures and implementing timely interventions. Advances in diagnostic tools have made it possible to assess bone density precisely, identifying individuals at risk long before a fracture occurs. These tools provide valuable insights, guiding tailored treatment plans.
The gold standard for diagnosing osteoporosis is the Dual-energy X-ray Absorptiometry (DXA or DEXA) scan. This non-invasive test measures bone mineral density (BMD) at key sites, typically the hip and spine, which are common locations for osteoporotic fractures. The results are reported as T-scores, comparing an individual’s BMD to that of a healthy young adult reference population. A T-score of -2.5 or lower indicates osteoporosis, while scores between -1.0 and -2.5 suggest osteopenia, a precursor to osteoporosis.
Beyond the DXA: Complementary Diagnostic Tools
While DXA remains central, other diagnostic approaches offer additional insights, particularly in assessing fracture risk and monitoring treatment effectiveness. These include:
- FRAX Tool: The Fracture Risk Assessment Tool (FRAX) is a computer-based algorithm that calculates an individual’s 10-year probability of suffering a major osteoporotic fracture (hip, spine, forearm, or shoulder). It integrates BMD T-scores with clinical risk factors like age, gender, body mass index, previous fractures, parental history of hip fracture, current smoking, alcohol consumption, and use of oral corticosteroids.
- Quantitative Computed Tomography (QCT): QCT provides a 3D assessment of BMD and can distinguish between trabecular and cortical bone, offering a more detailed analysis of bone structure. While not as widely used as DXA for routine screening, it can be beneficial in certain complex cases.
- Bone Turnover Markers (BTMs): Blood and urine tests can measure biochemical markers related to bone formation and resorption. While not diagnostic of osteoporosis themselves, BTMs can provide insights into the rate of bone remodeling and can be used to monitor the effectiveness of anti-resorptive therapies.
The interpretation of these diagnostic results requires the expertise of healthcare professionals, who can integrate the findings with an individual’s overall health history and lifestyle. The goal is not just to diagnose osteoporosis but to understand the specific factors contributing to an individual’s bone weakness and to develop a comprehensive, personalized management plan. Regular screening, especially for women over 65 and men over 70, or those with significant risk factors, is crucial. Proactive diagnostic efforts empower seniors and their healthcare providers to intervene early, dramatically reducing the likelihood of debilitating fractures. This proactive approach underscores the shift from treating fractures to actively preventing them.
Comprehensive Prevention: A Holistic Approach
Preventing osteoporosis and subsequent fractures in seniors is a multifaceted endeavor that transcends simple calcium intake. It necessitates a holistic approach, integrating lifestyle modifications, nutritional considerations, and, when appropriate, pharmacological interventions. This comprehensive strategy aims to build and maintain bone density, improve balance, and reduce fall risk.
At the core of prevention lies a commitment to physical activity. Weight-bearing exercises, such as walking, jogging, stair climbing, and dancing, are particularly effective as they stimulate bone formation by placing stress on the bones. Strength-training exercises, using weights or resistance bands, also play a crucial role by improving muscle strength and balance, thereby reducing the risk of falls, a primary cause of osteoporotic fractures. For seniors, exercises that improve balance, such as Tai Chi, are equally important. These activities not only fortify bones but also enhance coordination and stability, minimizing the likelihood of injurious falls.
Dietary Cornerstones: Building Stronger Bones from Within
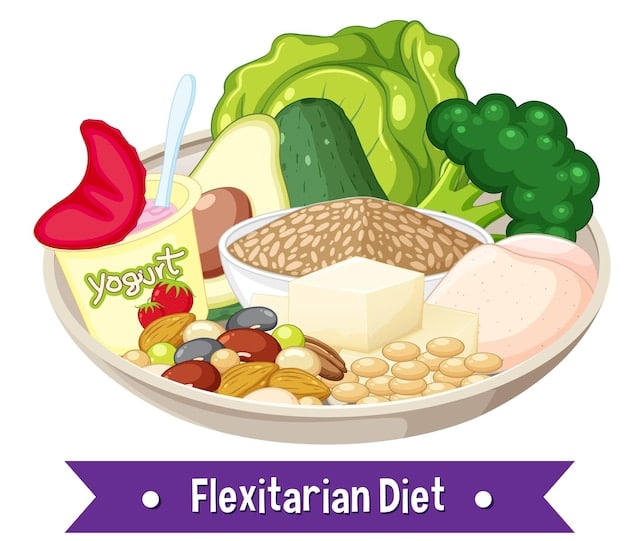
Nutrition forms another critical pillar of osteoporosis prevention. While calcium and vitamin D are widely recognized for their importance, a balanced diet rich in other essential nutrients also contributes to bone health.
- Calcium: Adequate calcium intake is fundamental. Recommended daily allowances for seniors are typically 1,200 mg. Good sources include dairy products, leafy green vegetables (kale, broccoli), fortified cereals, and salmon.
- Vitamin D: Essential for calcium absorption, vitamin D can be obtained through sun exposure, certain foods (fatty fish, fortified milk), and supplements. Seniors often require higher doses, with recommendations typically ranging from 800-1,000 IU daily.
- Other Nutrients: Magnesium, phosphorus, vitamin K, and protein also play roles in bone metabolism and density. A varied diet emphasizing fruits, vegetables, lean proteins, and whole grains supports overall bone health.
Beyond diet and exercise, lifestyle modifications can significantly impact bone density and fracture risk. Avoiding smoking and excessive alcohol consumption is crucial, as both are detrimental to bone health. Smoking reduces bone mass and interferes with calcium absorption, while excessive alcohol intake can impair bone formation and increase fall risk.
For some seniors, particularly those with existing osteopenia or osteoporosis, healthcare providers may recommend pharmacological interventions. These medications, which include bisphosphonates, selective estrogen receptor modulators (SERMs), and anabolic agents, work in various ways to slow bone loss, increase bone density, or stimulate new bone formation. The choice of medication is highly individualized, based on an assessment of fracture risk, bone density, and other health considerations.
Implementing these preventive strategies requires a proactive mindset and consistent effort. Regular consultations with healthcare providers, including bone density screenings, are essential for monitoring bone health and adjusting prevention plans as needed. By embracing a comprehensive approach, seniors can significantly reduce their risk of osteoporosis and enjoy a more active, independent life free from the burden of fractures.
Navigating Pharmaceutical Options: A Detailed Look
When lifestyle and nutritional strategies alone aren’t sufficient to manage osteoporosis, pharmaceutical interventions become a critical component of treatment. The landscape of osteoporosis medications has evolved, offering various options tailored to individual needs and severity of bone loss. Understanding these options is essential for informed decision-making in consultation with a healthcare provider.
The primary goal of pharmacological treatment is to prevent fractures by slowing bone loss, increasing bone density, or stimulating new bone formation. The most commonly prescribed medications fall into several classes, each with distinct mechanisms of action and administration methods.
Classes of Osteoporosis Medications
The choice of medication depends on several factors, including the patient’s bone mineral density, history of fractures, other medical conditions, and specific risk factors. Each class of medication offers unique benefits and potential side effects.
- Bisphosphonates: These are often the first-line treatment. They work by slowing down the bone resorption process, preserving existing bone and modestly increasing bone density. Common bisphosphonates include alendronate, risedronate, ibandronate, and zoledronic acid. They can be taken orally (daily, weekly, or monthly) or intravenously (quarterly or annually).
- Denosumab (Prolia): This is a monoclonal antibody administered as an injection every six months. It targets a protein crucial for bone breakdown, effectively reducing bone resorption and increasing BMD. It is often considered for those who cannot tolerate bisphosphonates or have kidney issues.
- Selective Estrogen Receptor Modulators (SERMs): Raloxifene is a SERM that acts like estrogen in some tissues (including bone) but not in others. It helps prevent bone loss and can lower the risk of spinal fractures in postmenopausal women.
- Anabolic Agents: Unlike antiresorptive drugs, anabolic agents stimulate new bone formation. Teriparatide (Forteo) and abaloparatide (Tymlos) are parathyroid hormone analogs given daily by injection, typically for a limited duration (e.g., two years). Romosozumab (Evenity) is another anabolic agent that combines bone formation stimulation with bone resorption inhibition, administered monthly by injection for up to 12 months. These are usually reserved for severe cases or those at very high fracture risk.
- Calcitonin: Available as a nasal spray or injection, calcitonin is a less potent option, often used for pain relief after a spinal fracture and for women who are five years past menopause.
While these medications are highly effective in reducing fracture risk, they are not without potential side effects. Bisphosphonates, for example, can cause gastrointestinal issues, and in rare cases, osteonecrosis of the jaw or atypical femoral fractures. Denosumab requires careful monitoring to prevent hypocalcemia. Patients must discuss the benefits and risks of each medication with their healthcare provider to determine the most appropriate and safest treatment plan for their individual circumstances. Adherence to the prescribed regimen is crucial for maximizing therapeutic benefits and preventing debilitating fractures, allowing seniors to maintain their independence and quality of life.

Fall Prevention: A Critical Layer of Protection
While strengthening bones is paramount in managing osteoporosis, an equally crucial aspect of fracture prevention in seniors is mitigating the risk of falls. A significant majority of osteoporotic fractures, particularly hip fractures, occur as a direct result of falls. Therefore, a comprehensive strategy must address factors contributing to falls and implement proactive measures to create safer environments and improve balance.
Falls in seniors are multifactorial, often stemming from a combination of intrinsic (individual-related) and extrinsic (environment-related) factors. Intrinsic factors include age-related declines in balance, muscle strength, vision, and sensation; chronic medical conditions such as Parkinson’s disease, arthritis, and neuropathy; and certain medications that can cause dizziness or drowsiness. Extrinsic factors involve hazards within the home or outdoor environment, such as slippery surfaces, poor lighting, loose rugs, and obstacles.
Implementing Effective Fall Prevention Strategies
Addressing these factors requires a targeted approach, encompassing medical review, physical activity, home modifications, and sensory aids.
- Medication Review: Regularly reviewing all medications with a healthcare provider is essential. Some drugs, or combinations thereof, can cause side effects like dizziness, confusion, or postural hypotension, increasing fall risk. Adjustments or alternatives might be necessary.
- Strength and Balance Training: Engaging in exercises specifically designed to improve strength and balance is incredibly effective. Tailored programs such as Tai Chi, specific balance exercises, or physical therapy can significantly enhance stability and reduce fall incidence.
- Home Safety Modifications: Simple yet effective changes to the living environment can dramatically reduce fall hazards. This includes removing loose rugs, ensuring adequate lighting, installing grab bars in bathrooms, adding handrails to staircases, and de-cluttering walkways.
- Vision and Hearing Checks: Regular eye and ear examinations are vital. Vision impairment can obscure obstacles, while hearing loss might prevent an individual from noticing approaching hazards or warnings. Updated prescriptions for eyeglasses and hearing aids can make a significant difference.
Additionally, wearing appropriate footwear with good support and non-slip soles, and being mindful of walking surfaces, especially outdoors, further contribute to fall prevention. For some seniors, assistive devices like walkers or canes may become necessary and, when used correctly, can provide essential support and stability, greatly reducing the risk of a fall. The collaboration between seniors, their families, and healthcare providers is key to identifying individual fall risks and implementing a personalized prevention plan. By proactively addressing these risks, we can significantly protect seniors from the devastating consequences of osteoporotic fractures, fostering continued independence and a higher quality of life.
Lifestyle Adjustments: Enhancing Bone Resilience
Beyond clinical treatments and direct fall prevention, a proactive engagement with certain lifestyle adjustments can profoundly influence bone health and contribute to the overall resilience of the skeletal system in seniors. These daily choices, often seemingly minor, accumulate over time to create a significant protective effect against osteoporosis progression and related fractures.
One primary area of focus is ensuring adequate sleep and stress management. Chronic stress and insufficient sleep can disrupt hormonal balances, including those that regulate bone turnover. Prioritizing 7-9 hours of quality sleep per night and adopting stress-reduction techniques like meditation, deep breathing exercises, or gentle yoga can support overall physiological well-being, which indirectly benefits bone health. A well-rested body is also less prone to accidental falls due to improved coordination and alertness.
Holistic Well-being: Beyond Diet and Exercise
While diet and exercise are foundational, other aspects of daily living contribute significantly to bone resilience and fracture prevention. These elements promote an overall healthier lifestyle that supports bone density.
- Maintaining a Healthy Weight: Both being underweight and overweight can negatively impact bone health. Being underweight has been linked to lower bone mineral density, while obesity can increase the risk of falls and complicates recovery from fractures. A balanced approach to weight management, supported by diet and exercise, is crucial.
- Sun Exposure and Vitamin D Synthesis: While supplements are often necessary for seniors, moderate sun exposure can naturally stimulate vitamin D production. Approximately 10-15 minutes of direct sunlight on unprotected skin, a few times a week, can be beneficial, always being mindful of skin cancer risk.
- Quit Smoking and Limit Alcohol: These are non-negotiable for bone health. Smoking has been repeatedly shown to decrease bone density and increase fracture risk, while excessive alcohol intake interferes with calcium absorption and increases fall risk. Support groups and medical interventions are available for those struggling to quit.
- Regular Health Check-ups: Regular medical evaluations allow healthcare providers to monitor bone health, adjust medication dosages if necessary, and identify any new risk factors for osteoporosis or falls. This ongoing dialogue ensures that preventive strategies remain relevant and effective.
Furthermore, staying socially active and engaged offers psychological benefits that can indirectly support physical health, including motivation for exercise and adherence to healthy habits. Participating in community groups, hobbies, or volunteer work can keep seniors mentally and physically active, contributing to general well-being and reducing the sedentary lifestyle that can compromise bone strength. By weaving these lifestyle adjustments into the fabric of daily life, seniors can empower themselves to proactively enhance their bone resilience, significantly reducing their vulnerability to osteoporosis and safeguarding their independence for years to come.
The Future of Bone Health: Innovations and Outlook
The field of bone health is continuously evolving, with exciting innovations on the horizon that promise more effective prevention, earlier diagnosis, and more targeted treatments for osteoporosis. These advancements offer hope for a future where fractures are less common and seniors can maintain robust skeletal health well into their later years.
One significant area of research is in understanding the genetic and molecular pathways involved in bone remodeling. This deeper understanding is paving the way for the development of highly specific drugs that can manipulate these pathways to either inhibit bone resorption more effectively or stimulate new bone formation more powerfully. Personalized medicine approaches are also gaining traction, where treatment decisions are guided by an individual’s unique genetic profile and response markers, moving beyond a one-size-fits-all approach.
Emerging Technologies and Predictive Models
Technological advancements are revolutionizing how bone health is assessed and managed. Beyond traditional DXA scans, new imaging techniques and predictive models are emerging.
- Advanced Imaging: High-resolution peripheral quantitative computed tomography (HR-pQCT) provides exquisite detail on microarchitecture and bone strength, offering a more nuanced understanding of fracture risk than BMD alone. While still primarily a research tool, its clinical utility may expand.
- Artificial Intelligence (AI) and Machine Learning (ML): AI algorithms are being developed to analyze large datasets from patient medical records, imaging scans, and genetic information. These algorithms can identify patterns and predict fracture risk with greater accuracy, potentially leading to earlier and more targeted interventions for high-risk individuals.
- Remote Monitoring and Wearable Devices: Wearable technologies that track activity levels, gait patterns, and even detect falls are becoming more sophisticated. This data can provide real-time insights into an individual’s fall risk and encourage adherence to prescribed exercise regimens. Remote monitoring allows healthcare providers to keep a closer eye on patient progress and intervene proactively.
- Stem Cell and Gene Therapies: Looking further into the future, research into stem cell therapies for regenerating bone tissue and gene therapies to correct genetic predispositions to osteoporosis holds immense promise. While these are still largely in experimental stages, they represent a potential paradigm shift in treating severe bone loss.
The integration of these innovations with existing best practices will undoubtedly transform the landscape of osteoporosis management. However, the core principles of prevention—adequate nutrition, regular exercise, fall prevention, and early diagnosis—will remain foundational. The future outlook for bone health is bright, characterized by increasingly precise and effective strategies that empower seniors to live full, active lives, free from the shadow of osteoporotic fractures. Continued research, public health initiatives, and individual diligence will collectively drive progress towards this healthier future.
| Key Point | Brief Description |
|---|---|
| 🦴 Bone Health Basics | Osteoporosis weakens bones, increasing fracture risk, especially in seniors. It’s a silent disease, often without symptoms until a fracture occurs. |
| 🔍 Early Diagnosis | DXA scans are key for early detection of bone loss. Tools like FRAX help assess future fracture risk based on density and lifestyle factors. |
| 🍎 Lifestyle & Prevention | Emphasis on calcium, vitamin D, weight-bearing exercise, and fall prevention is crucial. Quit smoking and limit alcohol for stronger bones. |
| 💊 Treatment Options | Medications like bisphosphonates and anabolic agents can significantly reduce fracture risk by slowing bone loss or promoting new growth. |
Frequently Asked Questions About Osteoporosis and Fractures
▼
Osteoporosis is often asymptomatic in its early stages, earning it the moniker “silent disease.” However, as bone mass continues to decrease, subtle signs might appear. These can include a gradual loss of height over time, a stooped posture accompanied by back pain (due to vertebral compression fractures), or easily fractured bones from minor falls or impacts that wouldn’t typically cause a break in healthy bones.
▼
Diet directly impacts bone health primarily through the intake of calcium and vitamin D, crucial for bone density and strength. Calcium is the main building block of bones, while vitamin D facilitates calcium absorption in the gut. Deficiencies can lead to weak, brittle bones. Other nutrients like magnesium, vitamin K, and protein also play supportive roles in maintaining bone metabolism, underscoring the importance of a balanced diet.
▼
Weight-bearing exercises, such as walking, jogging, dancing, and climbing stairs, are most beneficial for bone health because they stimulate bone formation. Strength-training exercises, using weights or resistance bands, improve muscle strength and balance, significantly reducing fall risk. Balance-specific exercises like Tai Chi are also highly effective, enhancing coordination and stability to prevent injurious falls in older adults.
▼
Yes, the field of osteoporosis treatment is continually advancing. Beyond traditional medications like bisphosphonates, newer options include anabolic agents (e.g., romosozumab, teriparatide) that actively stimulate new bone formation, rather than just slowing bone loss. Research into stem cell therapies and personalized genetic approaches is also ongoing, promising more targeted and potentially regenerative treatments in the future for severe cases of osteoporosis.
▼
Fall prevention is paramount in the overall management of osteoporosis, as a significant majority of osteoporotic fractures, especially hip fractures, result directly from falls. Even with strong bones, a severe fall can cause a break. Strategies like home safety modifications, balance exercises, medication reviews to reduce dizziness, and regular vision checks are crucial for minimizing fall risk and, consequently, preventing debilitating fractures in older adults.
Conclusion
Understanding and proactively addressing osteoporosis and fracture prevention is more critical than ever for seniors. By combining early diagnosis through advanced tools, embracing comprehensive lifestyle and nutritional strategies, judiciously utilizing pharmaceutical options, and focusing relentlessly on fall prevention, older adults can significantly bolster their bone health. The ongoing innovations in diagnosis and treatment provide a promising outlook, reinforcing the idea that maintaining strong, resilient bones throughout the aging process is an achievable goal, pivotal for an independent and vibrant quality of life.





